Dementia (A Personal Story)
This article is difficult to write. It’s deeply personal and I respect my family’s privacy. However, I’m putting pen to paper in the hope that what I’ve learned about dementia may help you or somebody you love. After all, over 5 million Americans are now diagnosed with Alzheimer’s disease and it’s the third cause of mortality in our country.
This piece is about the journey of my beloved father from wellness to dementia. It’s written both from my personal viewpoint of what it’s like to watch somebody you love experience this debilitating condition; it’s also based on the research I’ve done to investigate the causes of Alzheimer's (or dementia) and what hope there is for prevention or recovery.
You’ll discover what the experts in natural health currently recommend to reduce your risk or mitigate the expected health decline post-diagnosis. Plus, I’ll be sharing my personal strategies for coping with the heartbreak of seeing a loved one walk this path. I truly hope that you never have to do so.
But first, let’s go back to the very beginning, before we ever suspected that the early warning signs were telling us something wasn’t right…

Setting The Scene: About My Father
To understand how my father’s health began to unravel, it’s helpful to know a little bit about the type of man he’d always been.
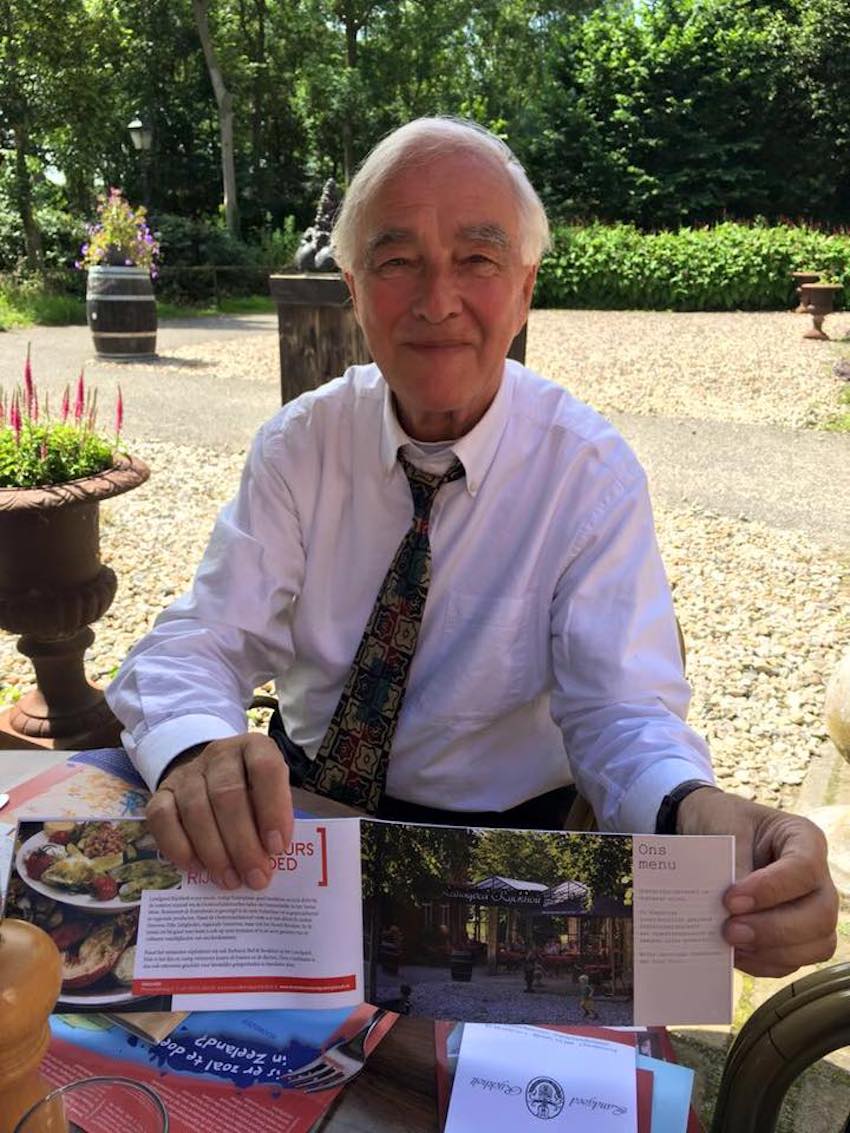
My father was a successful man in every material measure of that word. He was extremely driven, astute and ran multiple businesses across the world. He epitomized a businessman in so many ways; he was impeccably groomed, had beautiful, fine tastes in virtually everything - the type of gentleman who didn’t leave the house until his Italian leather shoes were buffed to a straight-out-of-the shoebox shine. He was truly a man of excellence, and I am eternally grateful for the opportunities he afforded us.
The point of me sharing this isn’t to boast about my father’s career. Rather, it’s to set the scene for the imminent changes that were uncharacteristic of this incredibly capable man.
About six years ago, my bright, detail-oriented father began to forget words when hewe would try to string a sentence together; names of close friends or family and even birthdays. The first time this happened, I brushed it aside as a memory lapse. We can’t remember everything all the time, right? However, as many more family birthdays were overlooked, it rang a few alarm bells. My father never forgot dates and family duties, plus other family members were also noticing changes. We started to worry.
With my father living so far away in my native country of Holland, it was difficult to gauge what exactly was going on. He was 65 years old, fiercely independent and living alone. So when the news arrived that my vader (“Father” in Dutch) had been diagnosed with dementia, it was still a deep shock. Every instinct cried out that I had to do something. When it’s someone you love, you’d do anything, right?
Dementia: A Degenerative Disease Of Toxicity
I began researching like a possessed woman. I was determined to find out why my father had dementia and more importantly, what I could do about it.
At Food Matters, we are blessed to be connected with some of the world’s best natural healers and repositories of natural health research. My quest for answers and hours upon hours of research has led me to reach a very convincing conclusion:
I believe that dementia is a degenerative disease of toxicity. Here’s why:
Mercury And Your Brain
My father has a mouthful of silver amalgam fillings. His teeth are literally riddled with them. Amalgam fillings are 50 percent mercury by weight! Mercury is a known neurotoxin and has absolutely zero place in the human body. Yet for decades my father had mercury next to one of his most precious organs, the brain. He refused earlier offers to have his fillings removed, and I believe that the toxins they released over the years contributed to his dementia.
Meat, Wheat and Sweets
What we eat directly affects the physiological functioning of our brain. A plant-rich diet supplemented with anti-inflammatory fats and high-quality proteins assists in the daily repair and cognitive processing of your brain. On the other hand, an ultra-processed, high-sugar diet deprives the brain of the essential nutrients it needs for optimal functioning and contributes to inflammation.
My father grew up in a culture and time in history where meat, wheat and sweets formed the basis of his diet. He’s Dutch, so dairy was always a given! But every meal was also centered around white bread of some description. We’d start the day with bread (loaded with butter and jam), then lunch with more white bread and ham. Dinner was typically more meat with starchy vegetables that were boiled into a barely-recognizable semblance of their original form. Yet to my father, this was never considered ‘unhealthy’. This was just the way everyone ate.
You’re probably noticing a bit of a discrepancy between how I was raised and the philosophies that we practise today at Food Matters. So you may be wondering: did I try to help my father to eat better?
You bet.
Yet my father came from a different generation where food represented different things. Ordering ‘water’ at restaurants was frowned upon as a status of poverty; in his view, we needed to support the economy and food industry by buying soda! Juicing was “too noisy”, smoothies were “too green” and green powders just didn’t taste good enough!
At the end of the day, my father was only really interested in his doctors’ advice.
However, not one medical practitioner ever raised the question of my father’s diet or suggested a lifestyle change to support his condition. Yet I’ve uncovered many nutritional factors that may help to prevent dementia or at least delay its progression:
The Gut/ Brain Connection
It’s no secret now that the state of our gut profoundly impacts the function of our brain. In fact, a significant portion of our brain’s neurotransmitters are actually made in the gut - a process that is influenced by the microbiome. Furthermore, it seems that the bacteria in the gut can even affect inflammation levels within the blood. In one recent study, probiotic supplementation of patients with Alzheimer’s reversed blood markers associated with this disease and improved several indices of cognitive performance.
Sugar: An Enemy To Your Brain’s Health
Scientists recognize that dementia involves some form of disordered glucose utilization in the brain. Furthermore, dementia and cognitive decline are also associated with beta-amyloid accumulation between neurons. These plaque-like buildups prevent signals from transmitting between neurons and create small restrictions in blood flow that cause inflammation and even cellular death.
Now here’s the really interesting part. Beta-amyloid directly competes with insulin degradation to get out of the brain. So if somebody has insulin resistance or has elevated levels of insulin in the brain from a high sugar diet, this reduces the ability of your brain to clear out beta-amyloid...the very stuff we know is related to the development of dementia.
Protein and Malnourishment
Upon diagnosis, over 50% of people with dementia report weight loss in the previous year. While that may sound appealing if you’d like to shed a few pounds, it’s actually quite alarming in the context of dementia.
When we lose weight, the body doesn’t merely break down fat tissue. We also lose some muscle mass. The degradation of muscle triggers a cascade of physiological events that ultimately elevates inflammation in the brain. This is associated with a significant decline in cognitive function among patients with dementia.
Despite the promise of these natural interventions to improve my father’s prognosis, why was nutrition never discussed by his medical team?
The Dangers Of Relying On Pharmaceutical Drugs
James and I tried our very best to persuade my father towards a healthier lifestyle, but our efforts over the years were futile. We met a solid wall of resistance. “Why should I listen to you?” We weren’t doctors, after all. My father obstinately refused our advice and put his full faith in medicine. This was final.
By his 70th birthday, my father’s condition progressed to a state whereby he was no longer able to live independently. The Dutch are extremely strict with this and there is a lot of government support to transition people into assisted living. So with a very heavy heart, James, Hugo and I flew back home earlier this year to help my father in this next phase of his journey.
It was very tough to accept the conditions of my father’s new reality. This bright, brilliant man who had worked so hard to enjoy a prosperous retirement was now denied many basic freedoms and pleasures in life. His facility operates like a military clock and my father is surrounded by many people who are far more advanced in their illness than he, which is morose to say the least. These weren’t the people, the routines, the freedoms he was used to. The food is heavily processed and devoid of the vital nutrients that I believe these people’s bodies are crying out for. And this was one of the ‘best’ institutions of its kind in Europe. My heart breaks to consider what other places might be like.
In this new environment, my father was frightened, angry and outspoken about his displeasure - as anybody would be. But instead of finding alternative ways to help him find calm and consolation, we were informed very matter-of-factly that he would need to be medicated. The insinuation was that this was to ‘keep the peace’.
The initial drugs my father was prescribed had terrible side-effects. He was sedated into a zombie-like state that left little of my father behind. I absolutely insisted that he was removed from these medications and had to fight long and hard to negotiate an alternative drug.
Today, he is taking a new pill called ‘quetiapine’. Here’s what drugs.com has to say about the side-effects of this medication:
“Quetiapine is an antipsychotic. It may increase the risk of death when used to treat mental problems caused by dementia in elderly patients. Most of the deaths were linked to heart problems or infection. Quetiapine is not approved to treat mental problems caused by dementia.”
Read that one more time. My elderly father, with dementia, is being treated with a drug that is explicitly known to cause problems - even death - in elderly patients with dementia.
I literally have no words to describe the emotion and anger that this incites in me. Yet our pleas for alternatives are stolidly ignored; we must, after all, ‘keep the peace’.

How To Deal With Dementia
First and foremost, as the old adage goes, prevention is far better than cure! I wholeheartedly encourage you and your loved ones to care for your beautiful bodies and reduce your risk of ever dealing with this devastating illness. Here are my top recommendations:
- DETOX. My research unequivocally convinces me that dementia is a degenerative disease of toxicity and in particular, heavy metal toxicity. So unless you breathe pure air, drink pristine water and live in isolation away from man-made chemicals, your body needs a little extra TLC to fully detoxify from modern assailants and run in tip top condition. James and I typically do a detox every three to six months.
-
DEAL WITH DENTAL AMALGAMS. I believe that mercury from amalgam fillings has been a big contributing factor to my father’s illness. If you have amalgam fillings, I encourage you to seek a holistic dentist who can safely remove these for you. I also urge you to find an integrative practitioner who can prescribe you a specialized heavy metal detoxification regime.
-
CARE FOR YOUR GUT. Courtesy of the gut-brain axis, when you look after your gut, you take care of your brain! Eat plenty of fiber, fermented foods, prebiotics, probiotics and resistant starch. Follow a low-sugar diet and minimize your intake of foods that harm your microbiota, such as coffee, alcohol and processed meat. Stressing less and sleeping more will also help out your gut health!
-
REDUCE INFLAMMATION. Most foods that are good for your heart are also good for your brain function, due to their systemic anti-inflammatory action. Good quality olive oil, ALA & DHA (found in walnuts, oily fish, chia, flaxseed/linseed), high-antioxidant produce and moderate amounts of cold-pressed coconut oil may all help to attenuate inflammation.
-
MOVE YOUR BODY. Physical exercise oxygenates your brain and has the wonderful benefit of lowering inflammation. Furthermore, resistance training can also help to retain muscle mass, which as we’ve seen earlier, is directly associated with a person’s rate of cognitive deterioration. People also tend to exercise socially, which has further benefits for reducing dementia risk.
How To Cope When Somebody You Love Has Dementia
For many of us, dealing with a dementia diagnosis is like losing a loved one but not being allowed to grieve.
When I visit my father, I see a soul that is trapped inside a body that is no longer serving him. I still see glimpses of the person he really is but those moments of recognition are slipping further and further away. It’s a slow grieving, as essentially we are already losing him - all those personality traits and quirks and things that make my Dad who he is - yet there’s no funeral or formal way to say goodbye. We say goodbye to pieces of him, instead.
The silver lining of the journey is that there are so many opportunities to make peace over past slights and hurts. We can also reminisce about the good times together and say the important things that people often leave too late to be said. When the final goodbye does arrive, we don’t need to have regrets. And that is a bigger blessing than many people get.
Secondly, I would gently encourage you to examine any guilt... and let go of it. Wholeheartedly. I struggled big time with this one, taking it upon myself to ‘cure’ my father. And while I certainly advocate for you to encourage your loved ones to follow the strategies we’ve talked about earlier, at some point you must also let go and accept that it’s not your burden to ‘fix’ them. Ultimately, we must accept that everyone is walking their own unique path through life and it’s not up to us to control that. Your guilt doesn’t change their situation, it only really hurts you.
So while my father is still in this world, I give thanks for the fact that I can still fly to Holland and give him a hug, enjoy his presence and celebrate the incredible life that he lived. He reminds me of the need to rejoice in each day that that we get to spend with the people we love and to never, ever, take our health and happiness for granted. In sharing this, I hope that you feel some measure of peace too.
Thank you for taking the time to read my story, and hopefully learn a little from the ups and downs that it’s held. Now, I’d love to hear from you!
Have You Ever Dealt With Dementia In Your Family?
Do You Have Something To Share That Could Possibly Help Somebody Else In This Position?
Discover how to eat your medicine to heal your gut, eliminate bloating, skin issues and hair loss as I share seven nutrition principles in this free masterclass. Running for a limited time only.